Cataract
A cataract is any opacity in our natural lens. You would think that opacity in the lens will cause visual problems but that is not entirely true. There are many types of cataracts, some affecting your eyesight very slowly but others, much faster. A cataract only needs surgical removal if it affects your eyesight significant enough to interfere with your daily living.
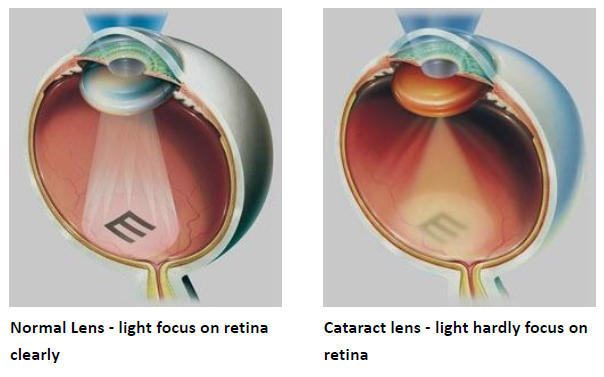
Some cataracts create no symptoms at all. Others lead to worsening nearsightedness or glare. The most common symptom is blurry vision.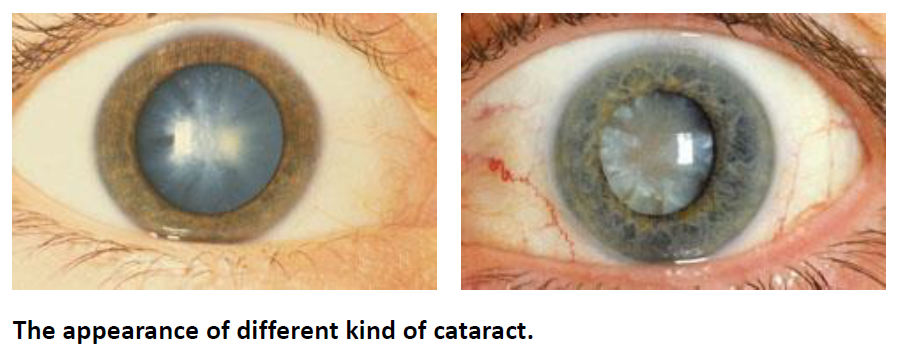
By the time a cataract is matured, an eye's vision is most probably very blurry. Certainly, a matured cataract can still be removed at this stage, but it is also true that removal is more difficult and potentially more hazardous. Corneal edema will be more severe and recovery of vision may take longer. Removal of a visually significant cataract before it reaches the mature stage is now advisable. However, what constitutes “visually significant” is not an unyielding rule. A safe rule of thumb is if your cataract does not bother your eyesight, you do not need to have it removed. If you are in doubt, you should undergo a full examination with your eye doctor. If you are still in doubt, seek more opinion from a different doctor.

"Phacoemulsification" refers to a modern and advanced technique to remove a cataract.
Basically, the central part of the human lens, called the nucleus, is relatively hard and cannot be removed by simple suction like drinking a Cola through a straw.
Therefore in the past, the surgeon would have to make a large opening and then "squeeze out" the nucleus. Having a large opening has several disadvantages. The eye can suddenly bleed profusely during surgery and become blind. A large opening creates potential for large amounts of astigmatism. Most patients undergoing this old type of surgeries need to wear glasses after the surgeries.
In phacoemulsification, the surgeon delivers ultrasound energy through a small probe. The ultrasound energy will convert the hard nucleus into millions of small particles – thus the term “emulsification”. The entire surgery can now be carried out with a very small opening. Visual recovery is relatively faster and patient has less astigmatism. A lot more patients who have undergone phacoemulsification can walk around without the use of eyeglasses.
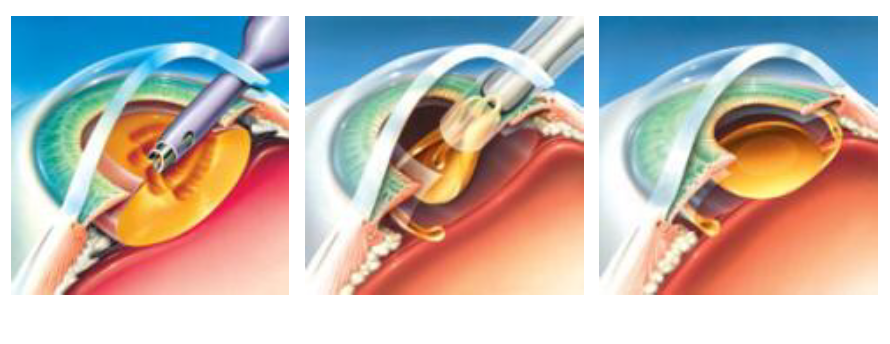
Through a small incision, use a small probe, The ultrasound energy will convert the hard nucleus into millions of small particles and remove them. Insert an intraocular lens & leave it inside the eye
After the surgeon removes a cataract, he usually inserts an intraocular lens. This is a precision-made plastic which replaces the original function of the natural lens – which is to focus light onto the retina

The focal point is elongated by using optical principles, so it provides a longer depth of focus than traditional monofocal intraocular lenses, thus providing better vision at both long and medium distances. It uses smaller optic rings or interval to produce a relatively long focal point, so the halo or glare phenomenon will be less than that of multifocal lenses. Doctors sometimes advocate monovision correction to reduce the patient's dependence on glasses.

Intraocular Lenses FAQ
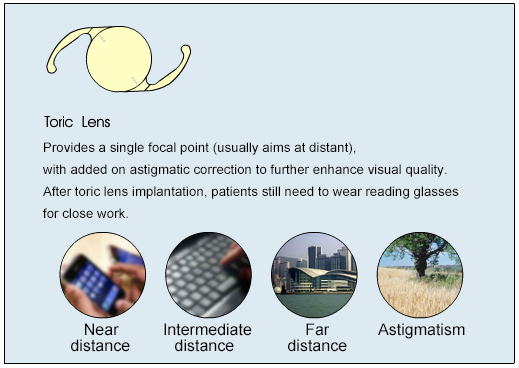
Astigmatism is a common refractive error due to uneven corneal curvature. Conventional intraocular lens could only correct long-sightness and short-sightness, but not astigmatism. Patients with astigmatism with conventional lens implants still need to wear glasses after the surgery. Nowadays, with the newly designed Toric Intraocular Lens, eye surgeons could also correct your pre-existing astigmatism during cataract surgery.
If you have minor astigmatism, or are happy using glasses to correct your astigmatism, you may not want or need to use toric intraocular lenses. If your astigmatism is more than 1 dioptre and do not want to wear astigmatic glasses, then you may consider using Toric Intraocular Lenses for cataract surgeries. However, for more than 5 dioptres of astigmatism, Toric Intraocular Lens alone may not achieve full correction and need to combine with other methods of astigmatism correction.
No. Toric lenses are monofocal lenses, they only correct your astigmatism, but not presbyopia. You will need reading glasses for close work.
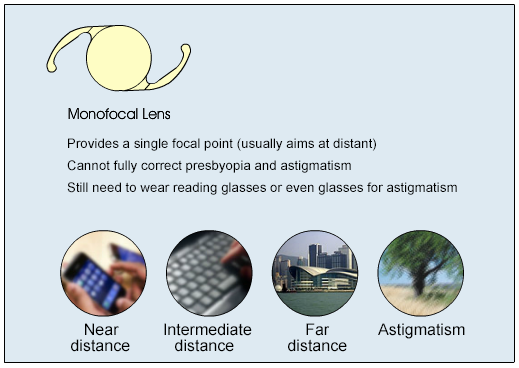
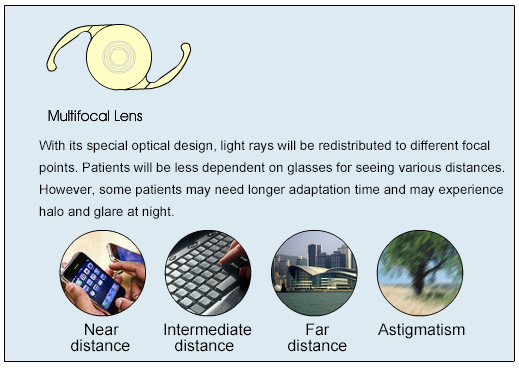
Traditional monofocal lenses focus light to only one point in space. A multifocal lens has more than one point of focus. A bifocal, which is a type of multifocal, has two points of focus, one at distance and the other at near.
A multifocal lens implant focuses light from distance and near simultaneously. This feature addresses both distant and near vision and makes the recipient less dependent on glasses or contact lenses. The implant provides reasonable good reading, intermediate and distance vision.
If you opt to receive a monofocal lens implanted in both eyes for distance vision, you will definitely need reading glasses after surgery. If you receive a multifocal lens there is a good chance you won’t need glasses. 80% of patients implanted with multifocal lenses in the FDA clinical trials did not need glasses after surgery for distance or near vision. Of course, not every patient in the trial was spectacle independent. The odds of becoming free of spectacles are better if your eyes are healthy.
25% of patients note glare and haloes around lights at night with the Multifocal Intraocular Lenses, a feature that is inherent to multifocal lenses. These effects may interfere with your ability to drive comfortably at night. However, most patients find that they get used to this phenomenon with time and the glare and haloes become less obvious. Night driving spectacles may assist in reducing this phenomenon. You should know that approximately 2-5% of patients implanted with monofocal lenses also notice glare and halos.
The surgical wound recovery from cataract surgery is the same whether you receive a monofocal lens or a multifocal lens. The brain must adjust, however, to the new optical system created with the multifocal lens. This neural adaptation takes from few days to months to occur. From our clinical experience, patients usually adapt better after the second eye surgery was performed.
No. It is recommended for most patients, but not for patients who have problems with their retina, advanced glaucoma, irregular corneal astigmatism, corneal diseases or optic neuropathy. If you are happy using reading glasses to correct your near vision, you may not want or need to use Multifocal Intraocular Lenses. In addition, your doctor will discuss the advantages and disadvantages of a multifocal lens as it pertains to your individual lifestyle and expectations. Patients with unrealistic expectations may not be appropriate for multifocal lenses.
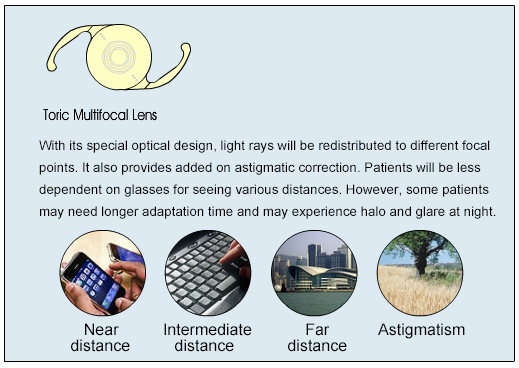
You don’t need and you can’t put in 2 intraocular lenses in one eye. Nowadays we have a newer type of lens that can combine both functions, called the Toric Multifocal Intraocular Lenses. The conventional type of multifocal lens implant could only be used in patients without astigmatism, but the Toric Multifocal lens serves to solve all refractive error in one goal. Similar to other multifocal lenses, these are not suitable for all patients, you need to discuss with your doctor first before making a decision.
Choosing an Extended Depth of Focus Intraocular Lens (EDOF) can be a viable solution. This lens has a longer depth of focus than traditional monofocal lenses, and has less halo or glare effect than multifocal intraocular lenses